Hey there, if you’ve stumbled upon the term “cholerhiasis,” you might be wondering what on earth it means. Well, relax—I’m here to break it down for you. Cholerhiasis is essentially another way to refer to the formation of gallstones, those pesky little hardened deposits that can crop up in your gallbladder or bile ducts. It’s a condition that’s more common than you might think, affecting millions worldwide, but it’s not always a big deal. In this guide, we’ll dive into everything from what causes it to how to handle it, all in a laid-back style while keeping things accurate and evidence-based. Think of me as your knowledgeable buddy who’s seen a lot of these cases. Let’s get started.
What is Cholerhiasis?
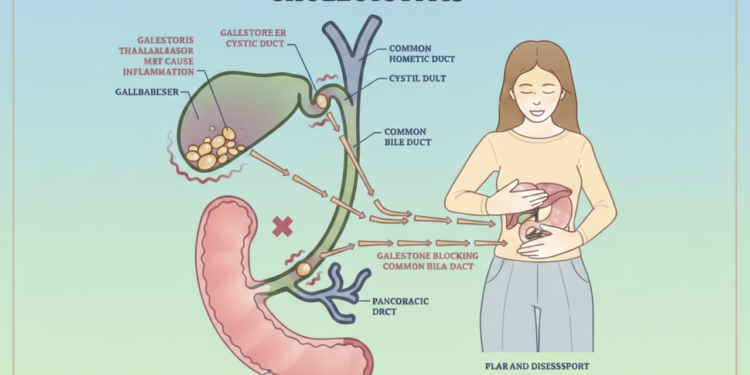
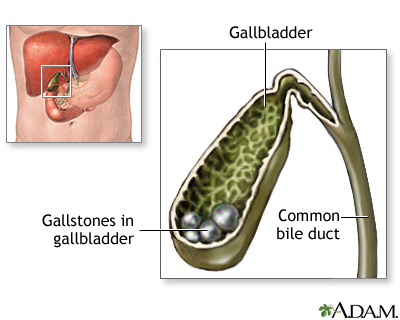
Cholerhiasis, often interchangeable with cholelithiasis in medical circles, describes the presence of stones made from bile components in the gallbladder or its connecting ducts. Your gallbladder is this small, pear-shaped sac tucked under your liver, acting like a storage tank for bile—a digestive juice your liver whips up to break down fats. When bile gets too concentrated or imbalanced, it can crystallize into these stones, ranging from tiny sand-like grains to golf ball-sized chunks. Most folks with cholerhiasis don’t even know they have it because it stays silent, but when it acts up, it can cause some real discomfort.
Diving deeper, these stones come in two main flavors: cholesterol stones, which are the yellowy ones making up about 80% of cases, and pigment stones, darker and linked to excess bilirubin from red blood cell breakdown. The term “cholerhiasis” might sound exotic, but it’s rooted in “chole” for bile and “lithiasis” for stone formation—basically, bile stones. It’s fascinating how something as simple as bile chemistry can lead to this, and while it’s not life-threatening on its own, understanding it helps you stay ahead of any issues.
In everyday terms, picture your gallbladder as a helpful sidekick in digestion. When everything’s balanced, bile flows smoothly to your small intestine after a meal. But with cholerhiasis, those stones can hang around harmlessly or decide to play blocker, disrupting the flow. Stats show about 10-15% of adults in the U.S. have them, with women twice as likely due to hormonal factors. It’s not something to panic about, but knowing the basics empowers you to listen to your body.
Causes of Cholerhiasis
At its core, cholerhiasis happens when your bile’s ingredients get out of whack. Bile is a mix of cholesterol, bile salts, and bilirubin, and normally, it stays liquid. But if there’s too much cholesterol—say, from your liver pumping out excess—or not enough bile salts to dissolve it, crystals form and grow into stones. This imbalance can stem from diet, genetics, or even how well your gallbladder empties. Rapid weight loss is a sneaky culprit too, as it floods your system with cholesterol from breaking down fat stores.
Let’s talk risk factors, because they’re key to understanding why some people get cholerhiasis and others don’t. Women, especially those who’ve been pregnant or on estrogen-based meds like birth control, are at higher risk because estrogen ramps up cholesterol in bile. Age plays a role—folks over 40 are more prone—and ethnicity matters, with Native Americans and Mexican Americans facing higher odds due to genetic predispositions. Obesity is a big one; extra body fat means more estrogen and cholesterol, plus it can slow gallbladder emptying, letting bile sit and concentrate.
Other triggers include certain medical conditions like diabetes, which affects fat metabolism, or liver diseases that mess with bilirubin levels. Even quick weight loss after bariatric surgery can spike your risk, as can low-fiber, high-fat diets that don’t encourage regular gallbladder contractions. It’s all about that delicate balance in your biliary system. If you’re nodding along thinking this sounds familiar, don’t worry—awareness is the first step to prevention, which we’ll cover later.
Symptoms and When to Seek Help
Many people with cholerhiasis cruise through life symptom-free, with stones just chilling in the gallbladder. But when a stone decides to move and block a duct, that’s when the party starts—or rather, the pain. The classic symptom is biliary colic: a sudden, sharp pain in your upper right abdomen, right under the ribs, that can radiate to your back or right shoulder. It often hits after a fatty meal, building up over minutes and lasting from 30 minutes to a few hours before easing off.
Nausea and vomiting can tag along, making you feel like you’ve got indigestion on steroids. If the blockage lingers, things escalate—fever, chills, jaundice (yellowing of skin and eyes), dark urine, or light-colored stools signal trouble like infection or inflammation. Women might experience this more subtly or chronically, sometimes dismissed as “just heartburn.” It’s your body’s way of saying, “Hey, something’s jammed up here!”
Knowing when to act is crucial. If pain lasts over five hours, spikes intensely, or comes with fever and jaundice, head to the ER— it could be a complication like cholecystitis. Even milder episodes warrant a chat with your doc, as recurring attacks mean the stones aren’t going away on their own. Listen to your gut (literally); early intervention keeps things from getting messy.
Diagnosis of Cholerhiasis
Diagnosing cholerhiasis is pretty straightforward once symptoms point that way. Your doctor starts with a chat about your history—any pain after meals? Family with gallstones?—followed by a physical exam, pressing on your abdomen for tenderness. Blood tests come next, checking for signs of infection, inflammation, or liver issues like elevated bilirubin or enzymes. These help rule out other culprits like ulcers or appendicitis.
The gold standard for spotting stones is an abdominal ultrasound—quick, painless, and non-invasive, it uses sound waves to visualize your gallbladder and ducts, catching most stones. If that’s inconclusive, especially for duct stones, they might go for a CT scan, MRI (like MRCP for detailed bile duct views), or a HIDA scan, which tracks bile flow with a radioactive tracer. Endoscopic ultrasound or ERCP can probe deeper, even removing stones during the procedure.
Accuracy is high with these tools, but sometimes stones are found incidentally during scans for other reasons. If you’re asymptomatic, no biggie—just monitor. But for symptoms, getting a clear diagnosis ensures the right treatment plan. It’s all about piecing together the puzzle without unnecessary pokes.
Treatment Options for Cholerhiasis
If your cholerhiasis is quiet, treatment might be zilch—just watchful waiting. But for bothersome stones, the go-to is cholecystectomy: surgical removal of the gallbladder. Don’t freak—it’s one of the most common surgeries, often laparoscopic with tiny incisions, meaning quicker recovery and less pain. You live fine without it; bile just flows straight from liver to intestines.
For those not surgery-ready—maybe due to other health issues—options include meds like ursodiol to dissolve small cholesterol stones over months or years, though recurrence is common. ERCP is handy for duct stones, using an endoscope to snag or crush them. In emergencies, like severe inflammation, a cholecystostomy tube drains the gallbladder temporarily.
Post-treatment, most folks bounce back fast. Laparoscopic surgery means home in a day, back to normal in a week or two. Some get loose stools from constant bile drip, but meds fix that. The key is addressing symptoms promptly to avoid complications—your doc will tailor it to you.
Prevention Strategies for Cholerhiasis
Preventing cholerhiasis boils down to lifestyle tweaks that keep your bile balanced. Maintain a healthy weight, but lose it gradually—aim for 1-2 pounds a week to avoid cholesterol surges. A diet rich in fiber from fruits, veggies, and whole grains helps, as does cutting back on high-cholesterol foods like fried stuff and red meat. Regular meals prevent bile from stagnating; skipping breakfast isn’t smart.
Exercise keeps things moving—30 minutes most days combats obesity and boosts gallbladder function. For at-risk groups, like women on hormones, chat with your doc about alternatives. If you’ve had weight-loss surgery, preventive meds might be prescribed. Hydration matters too; staying watered dilutes bile.
Long-term, these habits not only dodge stones but boost overall health. It’s not foolproof—genetics play a part—but stacking the odds in your favor feels good. Start small; even swapping soda for water counts.
Potential Complications of Cholerhiasis
While cholerhiasis is often benign, ignored stones can lead to drama. Cholecystitis—inflamed gallbladder from blockage—brings fever, severe pain, and needs antibiotics or surgery. If a stone slips into the common bile duct, choledocholithiasis causes jaundice and infection (cholangitis), risking sepsis if untreated.
Pancreatitis is another nasty one: a duct-blocked stone irritates the pancreas, causing intense abdominal pain and potential hospitalization. Rarely, chronic issues raise gallbladder cancer risk, though it’s super low. Perforation or abscesses are emergencies.
Spotting early signs prevents escalation. Regular check-ups if you’re high-risk help. Most complications are avoidable with timely care—don’t tough it out.
Living with Cholerhiasis
If you’ve got asymptomatic cholerhiasis, life rolls on—no changes needed, just awareness. For symptomatic cases pre-surgery, manage with low-fat meals to avoid triggers: think grilled chicken over burgers. Over-the-counter pain relief helps during attacks, but don’t rely on it long-term.
Post-cholecystectomy, adapt to “bile on demand”—some get diarrhea, eased by bile binders like cholestyramine. Diet stays important: high-fiber to regulate bowels. Stay active; it aids digestion.
Emotionally, it’s normal to worry, but most thrive without their gallbladder. Support groups or doc chats help. With cholerhiasis, knowledge is power—own it, and you’ll handle whatever comes.
Conclusion
Wrapping up, cholerhiasis—or gallstones, as it’s commonly known—is a manageable condition that affects many but troubles few. From understanding its bile-based origins to navigating treatments like surgery, you’ve got the tools to stay informed. Remember, most cases are symptom-free, and with lifestyle tweaks, you can minimize risks. If pain strikes, don’t hesitate to seek help—early action keeps things smooth. Stay healthy, listen to your body, and here’s to digestion without the drama!
(FAQs) About Cholerhiasis
1.) What exactly is cholerhiasis?
Cholerhiasis refers to the formation of gallstones in the gallbladder or bile ducts, hardened deposits from imbalanced bile components like cholesterol or bilirubin. It’s often asymptomatic but can cause pain if stones block ducts.
2.) How can I prevent cholerhiasis?
Prevention involves maintaining a healthy weight through gradual loss, eating a high-fiber, low-fat diet, exercising regularly, and avoiding skipped meals to keep bile flowing properly.
3.) What are the main symptoms of cholerhiasis?
Common symptoms include sudden upper right abdominal pain after meals, nausea, vomiting, and sometimes jaundice or fever if complications arise from blockages.
4.) Is surgery always necessary for cholerhiasis?
No, surgery is only needed for symptomatic cases; asymptomatic stones often require no treatment, though monitoring is advised to catch any changes.
5.) Can cholerhiasis lead to serious health issues?
Yes, if untreated, it can cause complications like gallbladder inflammation, bile duct infections, pancreatitis, or rarely, increased cancer risk, but prompt care prevents most problems.