Hey there, if you’ve ever noticed a weird spot, bump, or rash on your skin and wondered what the heck it is, you’re not alone. Primary skin lesions are basically the first signs your skin throws at you when something’s off—whether it’s a minor irritation or something that needs a doctor’s eye. As a dermatology enthusiast who’s spent years diving into the nitty-gritty of skin conditions, I’ll walk you through this in a way that’s easy to digest, without all the jargon overload. Think of this as your chill chat with a skin expert over coffee. We’ll cover what they are, the types, causes, how to spot them, treatments, and more. By the end, you’ll feel a bit more empowered about your skin’s signals.
What Are Primary Skin Lesions?
Primary skin lesions are the initial, unaltered changes that appear on your skin due to some underlying issue. Unlike secondary lesions, which evolve from primaries—like when a blister pops and turns into a crust—these are the fresh-out-of-the-box versions. They’re the skin’s way of saying, “Hey, pay attention!” without any scratching, picking, or time passing to change their look. Dermatologists love classifying them because it helps pinpoint what’s going on beneath the surface.
To break it down simply, imagine your skin as a canvas. Primary lesions are the first strokes: flat spots, raised bumps, fluid-filled sacs, you name it. They’re not caused by external trauma like cuts or burns; instead, they’re often tied to internal factors like infections, allergies, or autoimmune stuff. For instance, a macule is just a flat discoloration, smaller than a centimeter, like a freckle or a birthmark. But if it’s bigger, we call it a patch. The key is recognizing them early because they can be clues to bigger health puzzles.
Now, why do we care about these? Well, in my experience chatting with patients, ignoring a primary lesion can lead to complications. Take eczema— it often starts with red, itchy patches that are primary. Catch it early, and you can manage it with simple creams. Let it fester, and it might turn into something weepy and infected. Primary lesions are diverse, and understanding them isn’t just for docs; it’s for anyone who wants to take charge of their skin health. After all, your skin is your body’s largest organ, and it deserves some respect.
Common Types of Primary Skin Lesions
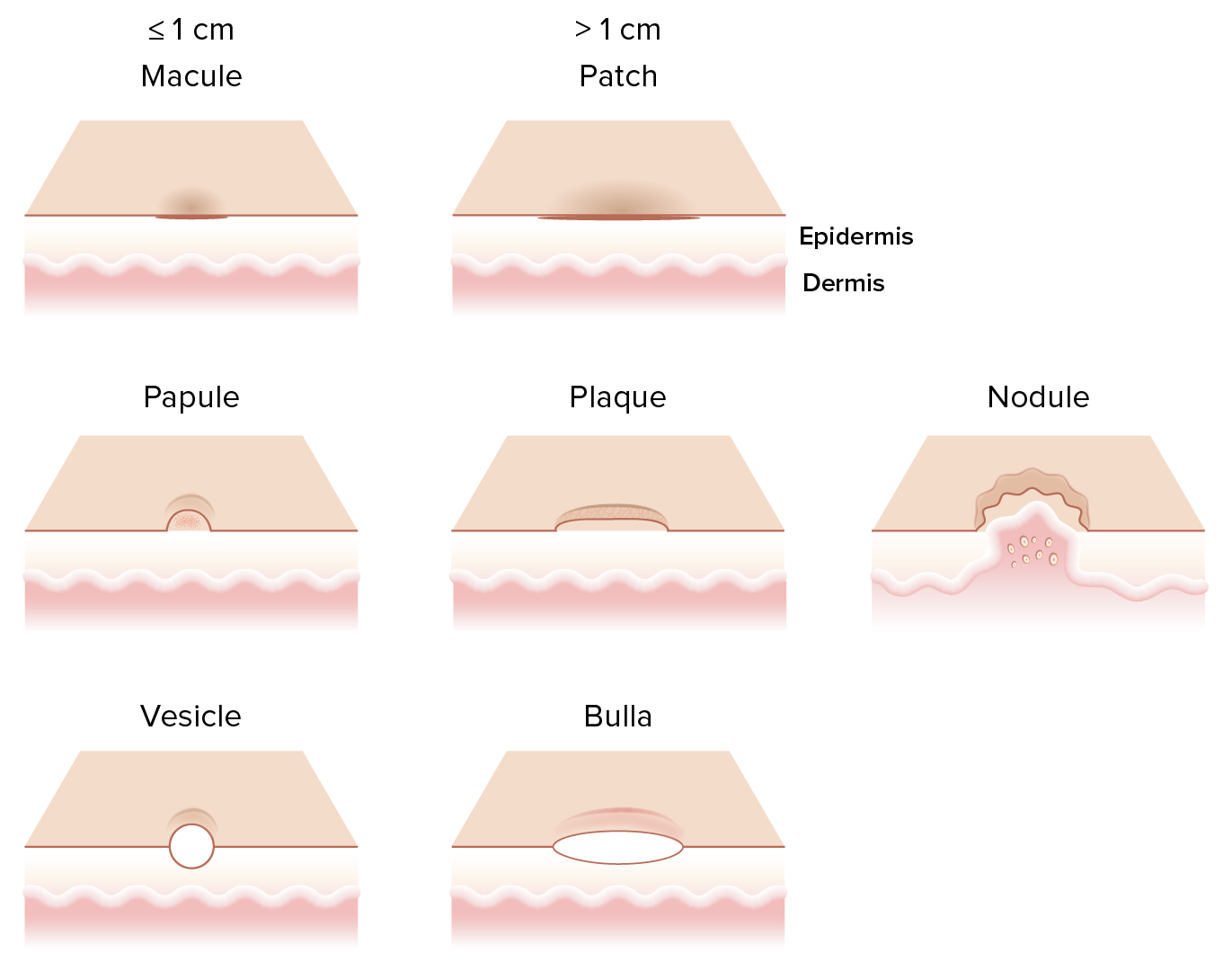
Let’s dive into the lineup of common primary skin lesions. First up are macules and patches, which are all about color changes without any texture shift. Macules are small, like those tiny red spots from petechiae after a hard cough, while patches are larger, think vitiligo where skin loses pigment in bigger areas. These are super common and often harmless, but sometimes they signal things like hormonal shifts or sun damage.
Next, we’ve got papules and plaques—the raised ones. Papules are small bumps, less than a centimeter, like acne pimples or insect bites. Plaques are bigger, flatter raised areas, often seen in psoriasis where they get scaly. I remember a case where a patient thought their plaque was just dry skin, but it turned out to be a fungal infection. The texture here is key; they’re solid, no fluid inside, and can itch or not, depending on the cause.
Then there are the fluid-filled crew: vesicles, bullae, and pustules. Vesicles are tiny blisters, like in herpes simplex or chickenpox, filled with clear fluid. Bullae are the big brothers, over a centimeter, seen in things like bullous pemphigoid. Pustules are pus-filled, think acne or folliculitis. These can be tricky because they might burst, turning primary into secondary, but spotting them fresh helps with quick treatment.
Don’t forget nodules and tumors, which are deeper and firmer. Nodules sit in the dermis, like in rheumatoid arthritis, feeling like hard lumps. Tumors are larger growths, benign or not, such as lipomas. And wheals? Those are the hives—edematous, itchy swells from allergies. Cysts are enclosed sacs, often sebaceous. Each type has its vibe, and knowing them lets you describe better to your doc.
Causes and Risk Factors for Primary Skin Lesions
Primary skin lesions don’t just pop up for fun; there’s usually a trigger. Infections are a biggie—bacterial like staph causing pustules, viral like HPV for warts (which are papules), or fungal like ringworm making annular plaques. Your immune system plays a role; if it’s wonky, you might see more lesions. Genetics can predispose you too, like in psoriasis where family history ups your risk.
Environmental factors are huge. Sun exposure? Hello, lentigines—those flat brown macules from UV damage. Allergens in your lotion or food can spark wheals or eczematous patches. Even stress can exacerbate things, turning a mild tendency into full-blown lesions. I’ve seen folks with nickel allergies get papules from jewelry, or latex from gloves causing vesicles. Lifestyle matters: poor diet, smoking, they weaken skin barriers, inviting trouble.
Certain groups are at higher risk. Kids often get viral lesions like molluscum contagiosum papules from playground shenanigans. Elderly folks might see more from thinned skin or meds. Diabetics? Watch for bullae or nodules due to poor circulation. Pregnancy can bring chloasma patches from hormones. Knowing your risks—like if you’re fair-skinned in a sunny climate—helps you stay vigilant and preventive.
Diagnosis and Evaluation of Primary Skin Lesions
Diagnosing primary skin lesions starts with a good look and chat. Dermatologists use the “look, feel, and ask” method: observe shape, size, color, distribution; palpate for texture, tenderness; and history for onset, changes, symptoms. Tools like a dermatoscope magnify details, spotting patterns invisible to the naked eye, like in melanoma macules.
Sometimes, tests are needed. Biopsies punch out a sample for lab analysis, confirming if a nodule is benign or not. Cultures swab pustules to ID bacteria or fungi. Blood tests check for systemic issues, like autoimmune markers in lupus erythematosus patches. Allergy testing pinpoints triggers for wheals. It’s not always invasive; often, a skilled eye suffices.
Evaluation considers the whole picture. Is it localized or widespread? Acute or chronic? Associated with fever or joint pain? This holistic approach avoids misdiagnosis—like mistaking a viral vesicle for bacterial. In my practice insights, patience is key; rushing can miss clues. Follow-ups track evolution, ensuring primaries don’t morph unchecked.
Treatment Options for Primary Skin Lesions
Treatment varies by type and cause, but the goal’s relief and resolution. For inflammatory ones like papules in acne, topical retinoids or benzoyl peroxide work wonders, reducing oil and bacteria. Steroids calm itchy plaques in eczema, applied sparingly to avoid side effects. Antivirals tackle vesicles in herpes, shortening outbreaks.
For infections, antibiotics zap bacterial pustules, antifungals ringworm plaques. Immune-modulators like biologics revolutionize psoriasis plaques for severe cases. Simple stuff helps too: moisturizers for dry patches, antihistamines for wheals. Surgery excises nodules or cysts if problematic, minimally invasive nowadays.
Holistic options? Diet tweaks reduce flare-ups in some, like gluten-free for dermatitis herpetiformis vesicles. Light therapy zaps certain plaques. Always tailor to individual—age, health, preferences. Monitoring prevents recurrence; education empowers self-care. With options galore, most primaries are manageable, restoring skin confidence.
Prevention and Care for Primary Skin Lesions
Prevention beats cure, right? Sun protection is non-negotiable—broad-spectrum SPF daily wards off UV-induced macules and patches. Hygiene habits curb infections: wash hands, avoid sharing towels to dodge viral papules. Balanced diet bolsters skin immunity, rich in vitamins A, C, E.
Allergen avoidance is key for prone folks—patch testing identifies culprits, preventing wheals or vesicles. Stress management via yoga or meditation tamps down flares in conditions like urticaria. Regular check-ups catch early lesions, especially if high-risk like diabetics monitoring for bullae.
Daily care routines matter: gentle cleansers, moisturizers maintain barrier, reducing irritation-prone plaques. Hydration inside-out helps. If traveling, adapt to climates—humid areas might spark more pustules, so pack accordingly. Empowering yourself with knowledge turns prevention into habit, keeping skin lesion-free.
In wrapping up this deep dive into primary skin lesions, remember they’re often benign signals, but listening to your skin can head off bigger issues. Stay curious, consult pros when unsure, and treat your skin kindly—it’s got your back, literally. Whether it’s a fleeting macule or persistent plaque, knowledge is your best defense. Thanks for hanging out with me on this skin journey; here’s to healthier, happier epidermis!
(FAQs) About Primary Skin Lesions
1) What exactly distinguishes primary skin lesions from secondary ones?
Primary skin lesions are the initial manifestations of a skin condition, appearing without any prior alteration, such as macules, papules, or vesicles. Secondary lesions evolve from primaries through processes like scratching, healing, or infection, examples being scales, crusts, or ulcers. The key is that primaries are the “starting point,” while secondaries show progression or interference.
2) Can primary skin lesions be a sign of something serious like cancer?
Yes, while many primary skin lesions are harmless, some can indicate underlying issues, including skin cancer. For instance, an irregular macule or patch might be an early melanoma, or a persistent nodule could be basal cell carcinoma. Always get unusual or changing lesions checked by a dermatologist to rule out serious conditions.
3) How can I tell if a primary skin lesion needs medical attention?
Look for the ABCDEs: Asymmetry, irregular Borders, varied Colors, Diameter over 6mm, and Evolving changes. Also, if it’s painful, bleeding, rapidly growing, or accompanied by symptoms like fever or fatigue, see a doctor. Better safe than sorry—early evaluation can make all the difference.
4) Are there home remedies that can help with common primary skin lesions?
Absolutely, for mild cases like allergic wheals, cool compresses or oatmeal baths can soothe. Tea tree oil might help acne papules, but dilute it to avoid irritation. However, these aren’t substitutes for professional advice; if lesions persist or worsen, consult a healthcare provider to avoid complications.
5) Do primary skin lesions affect all age groups the same way?
No, they vary by age—kids often get viral ones like chickenpox vesicles, teens battle acne papules from hormones, adults might see sun-related macules, and seniors deal with age spots or medication-induced lesions. Factors like immune strength and lifestyle influence how they present and resolve across life stages.